Obesity Is a Disease
Complications of Obesity
Obesity Is a Multisystem Disease Associated With Complications
Obesity gives rise to a wide range of complications that have a profound impact on multiple organ systems. Most of these complications are caused by the metabolic effects of adipose tissue, but some are caused by the mechanical effects of increased body mass or psychosocial effects. Often, these complications reduce the patient’s quality of life (QoL).1,2 Here is more information about obesity-related complications and how they may impact individuals with obesity.
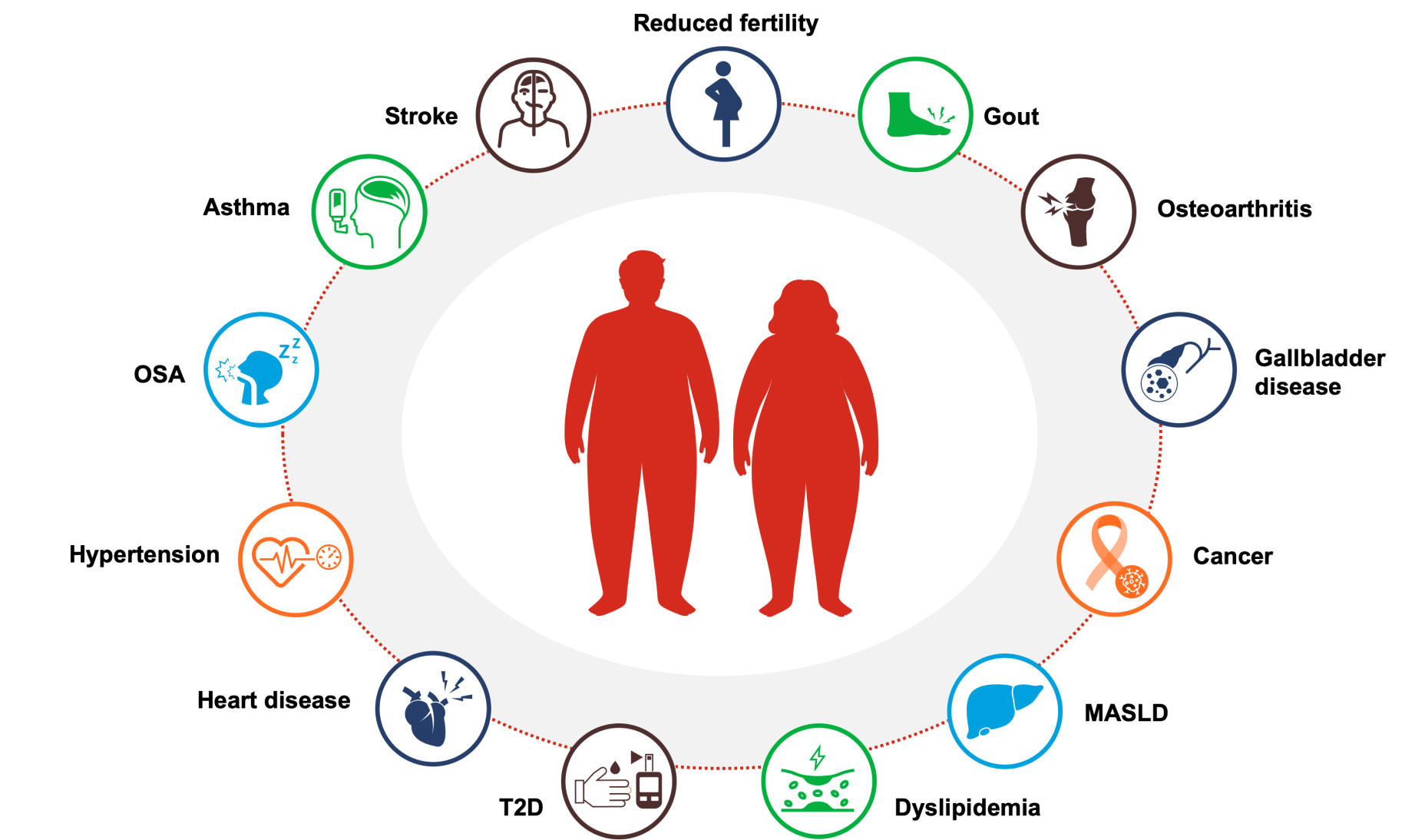
Stroke
Abdominal obesity is an independent, potent risk factor for ischemic stroke likely through its impact on lipids, blood glucose, blood pressure, or other cardiometabolic risk factors. It may increase the risk of ischemic stroke through vascular risk factors and other mechanisms, such as insulin resistance or metabolic syndrome.3
Obstructive Sleep Apnea (OSA)
Excess body fat has the potential to interfere with the mechanics of pulmonary physiology and is linked to several respiratory disorders, including OSA.4 A longitudinal study found that a 10% weight gain led to a 6-fold increase in the odds of developing moderate-to-severe OSA.5 OSA is common but often undiagnosed in people with obesity. In a retrospective study of patients presenting for bariatric surgery, the prevalence of OSA was 78%.6
Dyslipidemia
Dyslipidemia related to obesity is typically characterized by increased triglycerides, decreased HDL levels, and abnormal LDL composition. Dyslipidemia associated with obesity plays a major role in the development of atherosclerosis and cardiovascular disease.7
Hypertension
It is estimated that 78% of primary (essential) hypertension in men and 65% in women can be attributed to excess weight8. Individuals with obesity have a 3.5-fold increased likelihood of having hypertension.9
Heart Disease
Obesity is associated with an increased risk of developing heart disease, particularly heart failure (HF) and coronary artery disease (CAD).10 People with obesity are twice as likely to develop HF compared to those who have a healthy weight.11
Type 2 Diabetes (T2D)
Obesity, regardless of the genetic background, increases the risk of developing type 2 diabetes (T2D) by 8-fold or more.12
Reduced Fertility
The quantity and distribution of body fat affect reproductive function in women and men through a range of hormonal mechanisms. Women with obesity are at higher odds of infertility, miscarriage, and poor outcomes with assisted reproductive technology.13 In men, obesity is associated with poor sperm quality, lower testosterone level, and reduced fertility.14
Gout
About 4% of Americans have gout, and people with overweight or obesity are at a higher risk of developing gout. The association between obesity and gout may be related to metabolic effects, such as insulin resistance, which may in turn reduce renal urate excretion, resulting in increased levels of uric acid in the bloodstream.15
Osteoarthritis (OA)
Obesity and overweight increase the risk of OA of both weight-bearing and non-weight-bearing joints, such as the hands.16 A 5-unit increase in BMI is linked to a 35% higher risk of knee OA and an 11% higher risk of hip OA.17,18 Obesity may increase the risk of OA through biomechanical and metabolic pathways.19
Gallbladder Disease (GBD)
Obesity is a known risk factor for the development of gallstones, especially in women.20 This risk is increased with acute weight loss.21 Rapid weight loss may increase the risk of cholelithiasis. Adequate fat intake during weight reduction may reduce this risk.22
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD; formerly known as Non-Alcoholic Fatty Liver Disease [NAFLD]23)
The prevalence of MASLD is estimated to be 15-30% in the general population and 50-90% in people with obesity. Dysfunctional lipid handling in obesity may lead to ectopic fat deposition in the liver and other organs.24
Cancer
It is estimated that overweight and obesity in the United States account for 14% of all deaths from cancer in non-smoking men and 20% in non-smoking women.25 Overweight and obesity are associated with a higher risk of developing 13 types of cancer.26
Asthma
People with obesity have an increased risk of asthma, potentially mediated by metabolic, inflammatory, and biomechanical processes. The results from a meta-analysis show an odds ratio of incident asthma of 1.5 (with overweight versus lean group) and 1.9 (with obesity versus lean group). Results from several longitudinal epidemiological studies indicate that obesity often precedes incident asthma.27References
- Tsai AG, Bessesen DH. Obesity. Ann Intern Med. 2019;170(5):ITC33-ITC48.
- Sarma S, Sockalingam S, Dash S. Obesity as a multisystem disease: trends in obesity rates and obesity-related complications. Diabetes Obes Metab. 2021;23(Suppl. 1):3-16.
- Suk SH, Sacco RL, Boden-Albala B, et al. Abdominal obesity and risk of ischemic stroke: the Northern Manhattan Stroke study. Stroke. 2003;34(7):1586-1592.
- Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70-81.
- Peppard PE, Young T, Palta M, et al. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015-3021.
- Lopez PP, Stefan B, Schulmann CI, Byers PM. Prevalence of sleep apnea in morbidly obese patients who presented for weight loss surgery evaluation: more evidence for routine screening for obstructive sleep apnea before weight loss surgery. Am Surg. 2008;74(9):834-838.
- Howard BV, Ruotolo G, Robbins DC. Obesity and dyslipidemia. Endocrinol Metab Clin North Am. 2003;32(4):855-867.
- Hall JE, do Carmo JM, da Silva AA, et al. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116(6):991-1006.
- Kotchen TA. Obesity-related hypertension: epidemiology, pathophysiology, and clinical management. Am J Hypertens. 2010;23(11):1170-1178.
- Powell-Wiley TM, Poirier CP, Burke LE, et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021;143(21):e984–e1010.
- Kenchaiah S, Evans JC, Levy D, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347(5):305-313.
- Schnurr TM, Jakupović H, Carrasquilla GD, et al. Obesity, unfavorable lifestyle and genetic risk of type 2 diabetes: a case-cohort study. Diabetologia. 2020;63(7):1324-1332.
- Silvestris E, de Pergola G, Rosania R, et al. Obesity as disruptor of the female fertility. Reprod Biol Endocrinol. 2018;16(1):22.
- Katib A. Mechanisms linking obesity to male infertility. Cent European J Urol. 2015;68(1):79-85.
- Bai L, Zhou J, Zhou T, et al. Incident gout and weight change patterns: a retrospective cohort study of US adults. Arthritis Res Ther. 2021;23(1):69.
- King LK, March L, Anandacoomarasamy A. Obesity & osteoarthritis. Indian J Med Res. 2013;138(2):185-193.
- Jiang L, Tian W, Wang Y, et al. Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2012;79(3):291-297.
- Jiang L, Rong J, Wang Y, et al. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2011;78(2):150-155.
- Batushansky A, Zhu S, Komaravolu RK, et al. Fundamentals of OA. An initiative of Osteoarthritis and Cartilage. Obesity and metabolic factors in OA. Osteoarthritis Cartilage. 2022;30(4):501-515.
- Stender S, Nordestgaard BG, Tybjaerg-Hansen A. Elevated body mass index as a causal risk factor for symptomatic gallstone disease: a Mendelian randomization study. Hepatology. 2013;58(6):2133-2141.
- Weinsier RL, Ullmann DO. Gallstone formation and weight loss. Obes Res. 1993;1(1):51-56.
- Garvey WT, Mechanick JI, Brett EM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines for medical care of patients with obesity. Endocr Pract. 2016;22(Suppl. 3):1-203.
- De A, Bhagat N, Mehta M, et al. Metabolic dysfunction-associated steatotic liver disease (MASLD) definition is better than MAFLD criteria for lean patients with NAFLD. J Hepatol. 2023:S0168-8278(23)05044-4.
- Divella R, Mazzocca A, Daniele A, et al. Obesity, nonalcoholic fatty liver disease and adipocytokines network in promotion of cancer. Int J Biol Sci. 2019;15(3):610-616.
- Centers for Disease Control and Prevention. Obesity and cancer. https://www.cdc.gov/cancer/obesity/index.htm (Accessed May 11, 2023).
- Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625-1638.
- Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169-1179.
VV-MED-145555
Please rate your satisfaction with the content on the following statements:
Very Dissatisfied
Dissatisfied
Neutral
Satisfied
Very Satisfied