Obesity Is a Disease
Obesity Management: Goals and Barriers
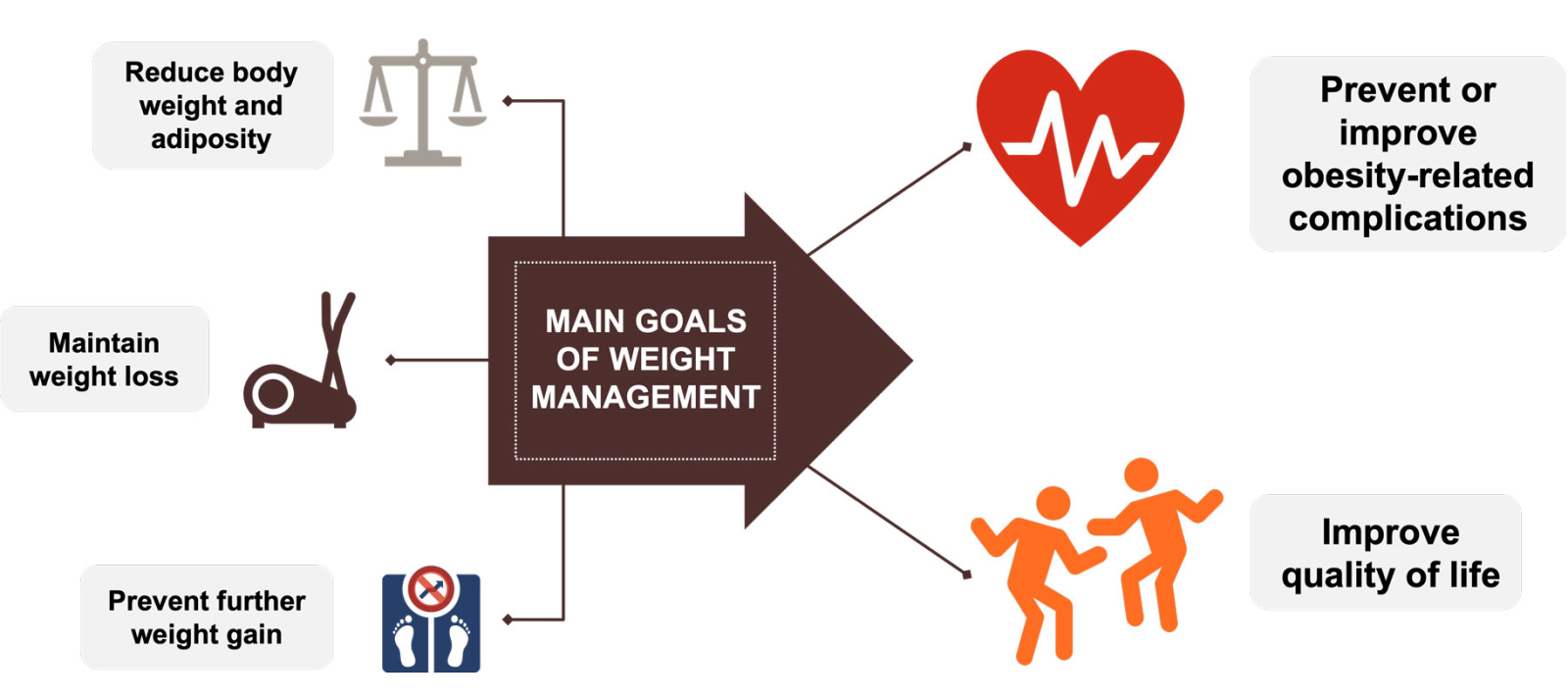
The main aims of obesity management include preventing or improving obesity-related complications and improving quality of life, which can be achieved through reduction of body weight, maintenance of weight reduction and prevention of further weight gain.

Biological Barriers
Weight reduction triggers adaptive changes in energy expenditure as well as hunger and satiety hormones, which persist over time and favor weight regain.2-4 Other factors which may influence response to obesity treatment include age, sex, genetic factors, presence of obesity-related complications, and use of certain medications5.
Barriers to Obesity Treatment: Views and Experiences of Patients and Clinicians
Patients report a variety of barriers to weight management, including weight bias in the healthcare setting.6 Clinicians also report challenges and barriers to providing care for patients with obesity, including gaps in education and training about obesity pathophysiology and available treatments, time pressures, and discomfort with navigating difficult conversations about weight.7 In the healthcare setting, there are many other barriers to weight management, including limited access to specialized obesity healthcare professionals and treatments,8 and other socioeconomic and environmental barriers, which limit access to healthcare,9 healthy food, and spaces for physical activity.10
Weight Bias and Stigma
Weight stigma refers to societal devaluation of people because of their body weight. At the root of weight stigma is weight bias, or prejudicial attitudes and inaccurate stereotypes about people with obesity, for example, that they lack the motivation or willpower to lose weight or that they are personally to blame for their weight. People living with obesity commonly experience weight bias and stigma in many areas of life, including healthcare. Weight bias can also be internalized; people with obesity may begin to hold negative beliefs about themselves due to their weight or size.6,11,12 The experience of weight bias can lead to psychological distress, physiological stress, disordered eating, and avoidance of physical activity, which can in turn impact weight and response to obesity treatment.13
Lack of Time During Office Visits
Lack of time during office visits is a frequently encountered barrier in obesity management. The average visit for an adult patient in the United States is about 20 minutes, with about 7 clinical items to be addressed.14 This greatly limits the time spent on discussing weight-related issues and weight management.15
Lack of Access to Specialized Obesity Healthcare Professionals and Treatments
Clinicians may have limited resources in their clinic to support patients engaged in obesity management.16 Fortunately, a variety of community-based organizations, such as TOPS17 (Take Off Pounds Sensibly) or the YMCA18 offer low-cost programs and resources to help support a healthy lifestyle. Patient-centered communication including specific, measurable, achievable, relevant, and time-bound (SMART)19 goal setting may help to engage a person with obesity during a visit.20
Ability to Access Clinical Care
When counseling a patient with overweight or obesity, social determinants of health should be considered as these can affect a patient’s access to healthcare, including obesity care.21 Other factors may impact patients’ ability to access care. For example, medical offices may not be well-equipped to accommodate patients with obesity. This can negatively affect patients’ experiences and contribute to future healthcare avoidance.13 In addition, health insurers may not cover anti-obesity therapies, requiring patients to pay out of pocket.22
Access to Healthy Foods
Various barriers limit access to and choice of healthy foods.23 These include environmental factors such as the availability of grocery stores and accessible transportation or targeted food advertising, economic barriers including the cost of healthy foods, time pressures and competing priorities, and cultural factors.23,24
Ability to Participate in Physical Activity
In many communities, individuals may not have access to safe and inexpensive opportunities for physical activity, including safe sidewalks, public parks, or recreation areas.10,24 The presence of weight-related complications, such as osteoarthritis or heart disease, may also impact an individual’s ability to participate in physical activity.15,25 In addition, patients who have experienced weight bias may not feel comfortable being active in public spaces.26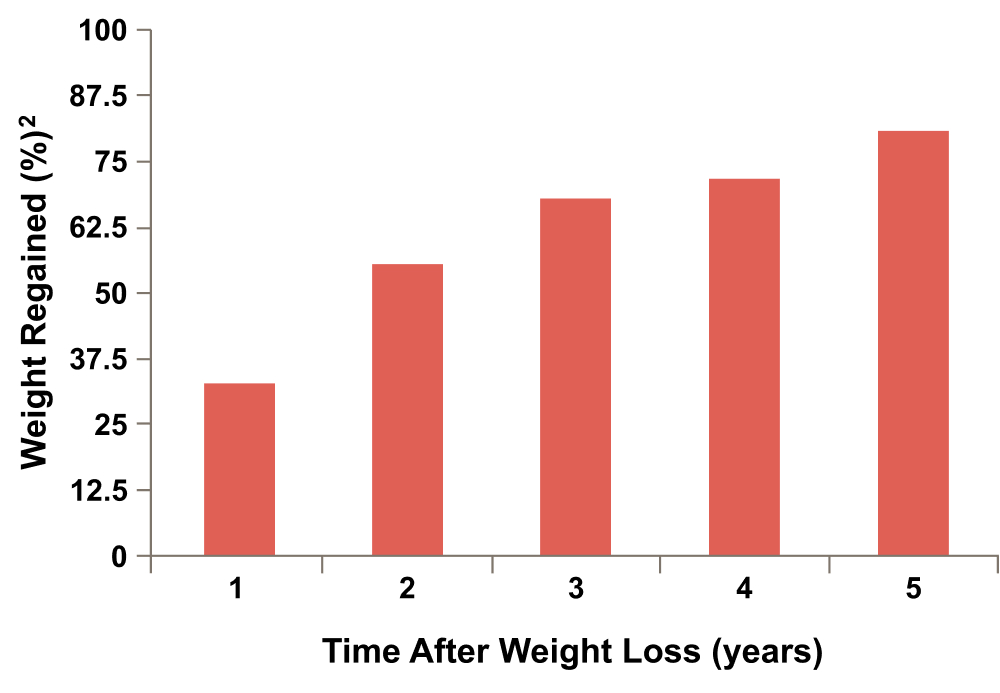
Maintenance of Weight Loss is Challenging and Weight Regain is Common
Individuals with obesity can achieve clinically meaningful weight loss (>5-10%) with lifestyle modifications,27 but weight regain is a common occurrence.1 A meta-analysis of 29 dietary interventions for obesity indicated that, within 4-5 years of initial weight reduction, an average individual regains most of the lost weight (~77%), thereby maintaining an average weight reduction of just 3% below the initial body weight.28 Even with structured, intensive lifestyle interventions and continual support, less than one-third of individuals are able to maintain weight reductions of ≥10% at 5-8 years.29,30References
- Wharton S, Lau DCW, Vallis M, et al. Obesity in adults: a clinical practice guideline. CMAJ. 2020;192(31): E875-E891.
- Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365(17):1597-1604.
- Fothergill E, Guo J, Howard L, et al. Persistent metabolic adaptation 6 years after "The Biggest Loser" competition. Obesity (Silver Spring). 2016;24(8):1612-9.
- Rosenbaum M, Hirsch J, Gallagher DA, Leibel RL. Long-term persistence of adaptive thermogenesis in subjects who have maintained a reduced body weight. Am J Clin Nutr. 2008;88(4):906-912.
- Dent R, McPherson R, Harper ME. Factors affecting weight loss variability in obesity. Metabolism. 2020;113:154388.
- Puhl RM, Lessard LM, Himmelstein MS, et al. The roles of experienced and internalized weight stigma in healthcare experiences: perspectives of adults engaged in weight management across six countries. PLoS One. 2021;16(6):e0251566.
- Simon R, Lahiri SW. Provider practice habits and barriers to care in obesity management in a large multicenter health system. Endocr Pract. 2018;24(4):321-328.
- Washington TB, Johnson VR, Kendrick K, et al. Disparities in Access and Quality of Obesity Care. Gastroenterol Clin North Am. 2023;52(2):429-441.
- Whitman A, De Lew N, Chappel A, et al. Addressing Social Determinants of Health: Examples of Successful Evidence-Based Strategies and Current Federal Efforts. ASPE Report. 2022
- Parise I. The built environment and obesity: you are where you live. Aust J Gen Pract. 2020;49(4):226-230.
- Kirk SFL, Salas XR, Alberga AS, et al. Canadian Adult Obesity Clinical Practice Guidelines. Reducing weight bias, in obesity management, practice and policy.
- Sabin JA, Marini M, Nosek BA. Implicit and explicit anti‐fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS One. 2012;7(11):e48448.
- Puhl RM. Weight Stigma and Barriers to Effective Obesity Care. Gastroenterol Clin North Am. 2023;52(2):417-428.
- Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23(12):2058-2065.
- Kim TN. Barriers to obesity management: patient and physician factors. J Obes Metab Syndr. 2020;29(4):244-247.
- Rhee KE, Kessl S, Lindback S, et al. Provider views on childhood obesity management in primary care settings: a mixed methods analysis. BMC Health Serv Res. 2018;18(1):55.
- Tops Club Inc.(R). Obesity Care and Support. https://tops.org/tops/TOPS/obesity-care-and-support.aspx (Accessed May 15, 2023).
- Schwartz RP, Vitolins MZ, Case LD, et al. Child Obes. 2012;8(6):577-582.
- Kris-Etherton PM, Petersen KS, Després JP, et al. Special Considerations for Healthy Lifestyle Promotion Across the Life Span in Clinical Settings: A Science Advisory From the American Heart Association. Circulation. 2021;144(24):e515-e532.
- Takahashi PY, Quigg SM, Croghan IT, et al. SMART goals setting and biometric changes in obese adults with multimorbidity: Secondary analysis of a randomized controlled trial. SAGE Open Med. 2019;7:2050312119858042.
- Munt AE, Partridge SR, Allman-Farinelli M. The barriers and enablers of healthy eating among young adults: a missing piece of the obesity puzzle: a scoping review. Obes Rev. 2017;18(1):1-17.
- Roser P, Bajaj SS, Stanford FC. International lack of equity in modern obesity therapy: the critical need for change in health policy. Int J Obes (Lond). 2022;46(9):1571-1572.
- Seguin R, Connor L, Nelson M, et al. Understanding barriers and facilitators to healthy eating and active living in rural communities. J Nutr Metab. 2014;2014:146502.
- Lee A, Cardel M, Donahoo WT. Social and Environmental Factors Influencing Obesity. [Updated 2019 Oct 12]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
- CDC. Arthritis as a potential barrier to physical activity among adults with obesity--United States, 2007 and 2009. MMWR Morb Mortal Wkly Rep. 2011;60(19):614-618.
- Thedinga HK, Zehl R, Thiel A. Weight stigma experiences and self-exclusion from sport and exercise settings among people with obesity. BMC Public Health. 2021;21(1):565.
- Pietrzykowska NB. Benefits of 5-10 Percent Weight-loss. OAC. 2013. https://www.obesityaction.org/wp-content/uploads/Benefits-of-5-10-Percet-Weight-loss.pdf (Accessed October 25, 2023).
- Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74(5):579-584.
- Wadden TA, Frey DL. A multicenter evaluation of a proprietary weight loss program for the treatment of marked obesity: a five-year follow-up. Int J Eat Disord. 1997;22(2):203-12.
- Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring). 2014;22(1):5-13.
VV-MED-145555
Please rate your satisfaction with the content on the following statements:
Very Dissatisfied
Dissatisfied
Neutral
Satisfied
Very Satisfied