Communication Toolkit for Alzheimer’s Disease
Communicating a Diagnosis
This page is part of a larger communication toolkit which provides general advice and best practices around communication of Alzheimer's disease (AD) in clinical practice.
See a full list of resources available on communicating a diagnosis of Alzheimer's disease.
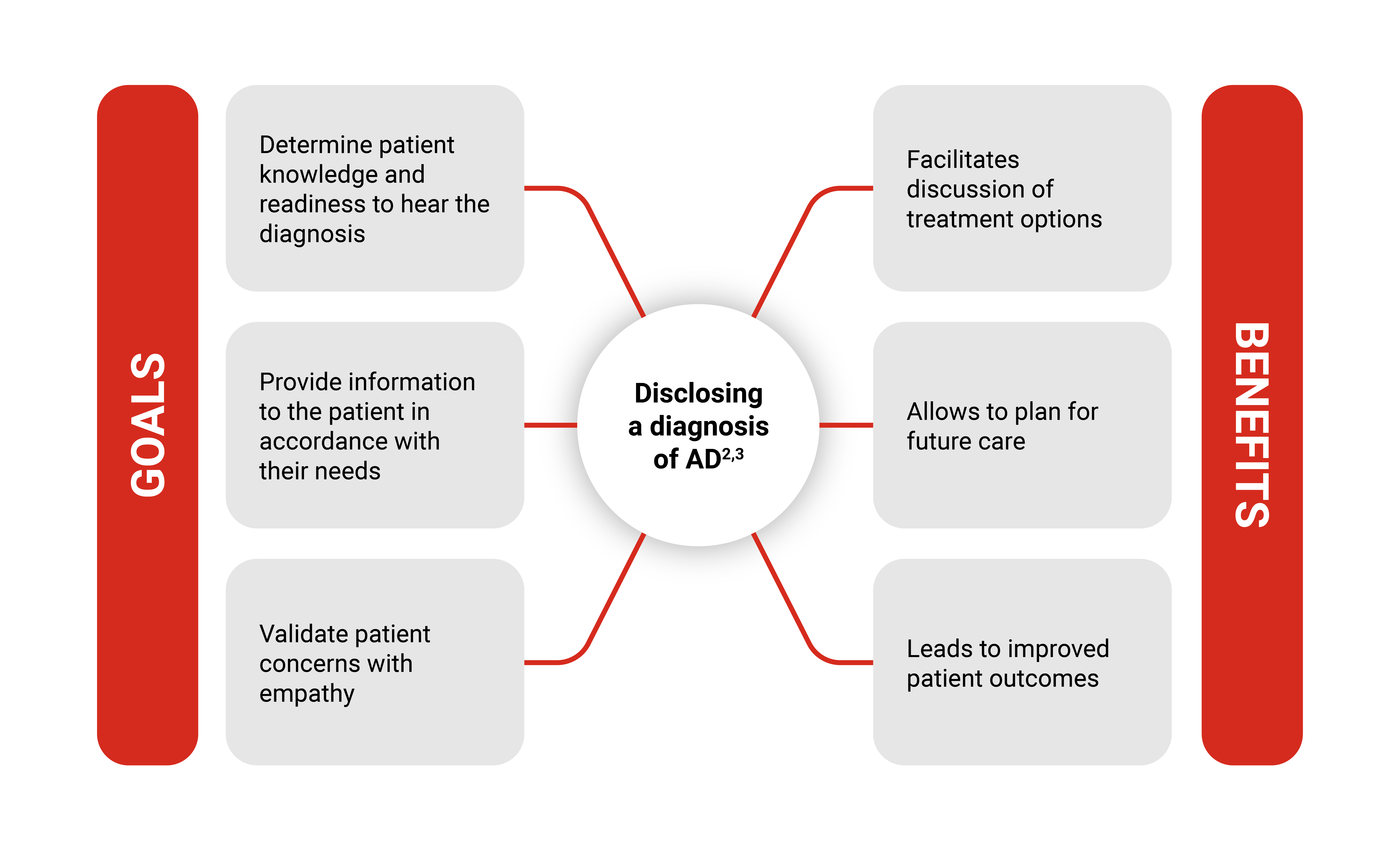
Graphic representation of key goals and benefits of disclosing a diagnosis of Alzheimer’s disease. Goals include determining patient knowledge and readiness to hear the diagnosis; providing information to the patient in accordance with their needs; and validating patient concerns with empathy. Disclosing a diagnosis of AD is beneficial, as it facilitates discussion of treatment options; allows to plan for future care; and leads to improved patient outcomes.
“The clinical diagnosis of AD should be a process rather than an event and can best be accomplished over the course of several visits. This strategy allows for more time to gather diagnostic information, assess the needs and capabilities of the patient and family (or other caregivers), and introduce the possibility of a diagnosis of AD gradually.”
-Grossberg et al, 20102
Move image slider tool for best practices rationale


Interactive element showing graphical representation of five best practices in communicating a diagnosis of AD. The first image panel details best practices in communicating a diagnosis of AD; moving the slider reveals a second image panel with corresponding benefits behind the identified best practices.
- Include at least one care partner: Care partners provide perspective on clinical history and support with future patient care.3
- Check patient understanding: Confirm patient understanding using tools such as the Teach Back method4,5
- Tailor the conversation to individual patient values and needs: Tailored conversations may encourage patient participation in shared decision-making3,4
- Actively practice empathy5: Step-up empathy language can enhance information sharing and foster trust5
- Ensure enough time: At least 15-20 minutes are required for the diagnostic Disclosure3
Recommendations for enhancing patient comprehension.3,4
- Use nonmedical terms and avoid jargon.
- Try to use mental/visual imagery wherever possible
- If the patient does not understand what you are saying, try saying it in a slightly different way instead
Recognize patient concerns.3,4
- Ask exploratory questions to understand
- In addition to the patient's words pay attention to their gestures, facial expressions, and tone of voice
Reassure the patient of your involvement.3,4
- Communicate to the patient and their loved ones that you are taking their concerns seriously
- Communicate willingness to act on the patient's behalf
Question #1
What communication strategy is emphasized as healthcare providers are communicating a diagnosis of Alzheimer’s disease to patients?
Option A:
Providing minimal information to avoid overwhelming the patient
Option B:
Utilizing technical medical jargon to convey the severity of the diagnosis
Option C:
Tailoring communication to the patient's cognitive abilities and emotional state
Related Resources
Downloadable PDFs
A powerpoint resource to enable HCPs to be better equipped to have a conversation with their patients about a diagnosis of Alzheimer’s disease (AD).
Music plays
Mr. Harris' memory has begun to exhibit signs of decline. Complicating matters is the knowledge that Mr. Harris's mother battled Alzheimer's disease.
Mr. and Mrs. Harris have met with Dr. Cohen about these concerns. She has administered a cognitive test, and requested some blood work and an MRI scan to exclude causes other than Alzheimer's.
Music plays
Today, Mr. Harris, and his wife, Jen, are meeting with Dr. Cohen to talk about the test results and seek further insight and guidance.
Music plays
Dr. Cohen: Mr. And Mrs. Harris, it's great to see you again. May I call you Jen and George? You were okay with that before?
Jen and George: Yes, of course.
Dr. Cohen: Yes? Okay. It's really good to see you. We were together a few weeks ago. We did some cognitive testing. You had some blood tests, and you had an MRI scan since I last saw you. So I want to go over all of those results, and then we can talk about next steps.
Dr. Cohen: How was the MRI?
George: Well, it's actually kind of noisy, you know, a little bit scary, you know, And you have to be like, really still, you know. So I had to go to the beach. I have to go somewhere or Hawaii or something.
Dr. Cohen: Yeah, you're picturing being on the beach. Good strategy. Good idea. You got through it. I'm glad.
Dr. Cohen: And I've got the results and we'll talk about that, okay?
Dr. Cohen: So just to recap how we got to this point, you had come to me not too long ago saying “something's going on with my memory. It's just not as reliable as it has been in the past. I'm still working.” You're in investments, correct?
George: Yes, yes.
Dr. Cohen: And you're still successful there and you're doing everything else for yourself, driving and shopping. And does he help with the cooking?
Jen: Yes, he does. He’s a good cook.
Dr. Cohen: Oh, he’s a good cook? Okay.
Dr. Cohen: So you're doing everything independently. And your sleep is good, your general health is good.
Dr. Cohen: And then you disclosed to me that mom had Alzheimer's- or we think it was Alzheimer's- in her seventies. So that sensitized you to the fact that there's something to check out here.
Dr. Cohen: So we did some cognitive testing together, and your score overall is quite good. You got 25 out of 30 on a test called the Montreal Cognitive Assessment- the MOCA for short- and that's a test of mild cognitive impairment.
Dr. Cohen: And it was just on the memory part of that that you had trouble. When we gave you five words, do you recall? And you were able to repeat them after me, but then after a distraction task, you could only come back with one of those five words. And that mirrors the memory problem you're noticing in day-to-day life.
Dr. Cohen: So I'm able to see what you're telling me about or what Jen's noticing. And the rest of the test, you did well. There's one other item that was tricky. It was copying a geometric figure. Do you remember that? The cube? It gave you some trouble?
George: Yeah. Yeah, it kind of- it gave me a little bit of trouble.
Dr. Cohen: Yeah. The perspective and the angles were a little wonky, so you lost a point on that. It's not, you know, a make-or-break thing. It just, again, gives us a little bit of a window into how the brain is working. But mainly it was the memory part that is telling me, ‘Yes, there is something going on’. You're noticing it. I can see it.
Dr. Cohen: We call this mild cognitive impairment- that's the syndrome diagnosis. But we need to dig deeper. What's causing it? Because I'm telling you what you already know- there's mild memory impairment- but this term, ‘mild cognitive impairment’, really refers to memory impairment or cognitive impairment while people are still functioning well and independently.
Dr. Cohen: So that that's you, as opposed to dementia, where people are no longer independent in all activities. So you did some blood work because we wanted to rule out things like thyroid disease or other things we can see in the blood that could cause memory problems.
Dr. Cohen: Your blood work is beautiful. That's good. So there's no deficiencies of any kind. B12 levels- good. As I said, the thyroid level, the cell counts, kidneys are functioning- all that's good. So, nice to have normal blood work. But we still need an answer. What's causing the memory problem?
Dr. CohenThen we did the MRI scan. And the MRI scan is nice. It's good. The structure of the brain looks good.
Jen: Good.
Dr. Cohen: That's a relief.
Dr. Cohen: No strokes, no tumors, no scars in the brain. Yeah. So, yeah, we want good news. We don't want to have tumors and strokes. That's good.
Dr. Cohen: No strokes, no tumors, no scars in the brain. Yeah. So, yeah, we want good news. We don't want to have tumors and strokes. That's good.
Dr. Cohen: But it's still not showing us that memory problem. And it still leaves open the possibility that Alzheimer's disease may be creeping up. And we want to rule that out, or be clear about whether that's what we're dealing with.
Dr. Cohen: So the next step to get greater confirmation on the diagnosis would be to send you for a scan called a PET scan. Okay? If you're willing to put up with another scan, it's not a noisy scan this time. It's not as tight or claustrophobic, but it is a scan. And it will give us a much clearer idea about specifically whether amyloid plaque is building up in the brain.
Dr. Cohen: And amyloid is a protein that starts accumulating in the brain very early in people who are developing Alzheimer's- even before symptoms. So it's a very, very early warning of Alzheimer's, and it's helpful to be clear about the diagnosis, because then that's the gateway to ‘how do we manage it, what do we do? How do we plan for the future? What treatments are relevant?’
Dr. Cohen: So if you're willing to go for this PET scan, that will give us good information to go forward with next steps. Does that sound okay?
George: Yeah. Yeah, it does. That sounds good.
Music plays
Mr. Harris completed the additional PET scan. Dr. Cohen requested. He and his wife now return to see the doctor and discuss the results of his full diagnostic evaluation.
Music plays
Dr. Cohen: George, Jen, great to see you again. Very glad to see you.
Dr. Cohen: So just to recap, we're here to talk about the PET scan results, and we talked about the fact that you have mild cognitive impairment. The MRI and the bloodwork weren't showing us the cause. We wanted to dig deeper and see “is this Alzheimer's disease?” So that's what we're here to talk about.
Dr. Cohen: So the PET scan does show this protein amyloid accumulating. And I know that's not what we were hoping for, but it is the reality that amyloid plaque is developing in the brain. And amyloid is that early, early change of Alzheimer's disease.
Dr. Cohen: So how are you doing with that now?
George: You know, I'm I was really hoping that there would be a different reason.
Dr. Cohen: That's very understandable.
George: But yeah, I had a feeling.
Dr. Cohen: You kind of felt that if it might show Alzheimer's and yet, of course, we're hoping for something else.
George: Yeah. Yeah. This- it's going to be- it's going to be difficult for me. You know- I don't want to forget about my kids. I don't want to forget about my grandkids.
Dr. Cohen: Of course, family is important and our memories are precious. Yeah.
Dr. Cohen: You know, this is a tough disease, Alzheimer's. But again, you've caught it early. And you're doing well day to day. The disease brings this cloud over your head. But our job now is to say, “let's live well, despite Alzheimer's”.
Dr. Cohen: Now that we know what this is, we could talk about treatment options, which we wouldn't be able to talk about very sensibly without having a diagnosis.
Dr. Cohen: And that's going to be important. And let's talk about, you know, bringing the family into the mix.
George: Yeah.
Dr. Cohen: Fortunately, as I said, you've caught this early, that gives us the best chance to try and keep this stable.
Dr. Cohen: When we talk about Alzheimer's disease, people often think right away of someone very disabled. Right. And they don't realize this is a very slowly progressive disease that starts almost imperceptibly. You know, where does normal aging end and Alzheimer's begin? A little bit of forgetfulness... You know, this is the very early, early stage.
Dr. Cohen: And we don't want him to feel less capable than he is. He's very capable. But we do also not want to ignore the diagnosis. So we'll talk more about the treatments that are possible. Okay. Okay. And I'll look forward to that detailed conversation. And you can decide if you want to bring your children in to join us. Okay?
Jen: Okay.
George: All right. Sounds good, Doctor.
Dr. Cohen: Okay. So, good to speak with you. And to be continued. Okay.
George: Thank you.
Dr. Cohen: You’re welcome.
Music plays
Communicating a Diagnosis of Alzheimer’s Disease with Mild Cognitive Impairment in Clinical Practice
Dr. Sharon Cohen demonstrates effective communication during the clinical assessment and a diagnosis of a patient living with Mild Cognitive Impairment from Alzheimer’s disease.
Music plays
Mrs. Olsen came to see Dr. Cohen because she started noticing problems with her memory and has increasingly relied on the caring assistance of her daughter, Debbie.
Music plays
In their first visit together, Dr. Cohen completed some brief cognitive assessments with Mrs. Olsen and requested some additional tests.
Music plays
Mrs. Olsen completed all the tests and is returning to see Dr. Cohen with her daughter, Debbie.
Music plays
Dr. Cohen: Hi, Mrs. Olsen. Great to see you again. Hi, Debbie. Thanks for coming. Appreciate it. How have you been since I last saw you?
Mrs. Olsen: Oh, I think I'm doing pretty good.
Dr. Cohen: Oh, good, good. I'm glad. Yes. You're checking with Debbie? Yes, She's doing okay.
Dr. Cohen: So we're here to talk about some test results. You had come to me a few weeks ago telling me about your memory not being so strong and worried that something was going on and you were having trouble paying your bills. So Debbie's been helping with that and having trouble remembering your medicine. So again, Debbie stepped up. She's helping. This is good. This is sensible.
Dr. Cohen: So we said, okay, let's see what we can find in the way of what's going on with memory. We did a test together, a paper and pencil test called the mini mental state exam, and we had you draw some pictures and repeat some words and various things. And your score on that test, it’s scored out of 30, and you got a score of 22 out of 30.
Dr. Cohen: So a lot of things you did well. But the things that were particularly challenging were the memory items. So knowing the exact date and remembering three words that we gave you to learn, but also a bit of trouble coming up with names of pictures. So it did show us on that test some of the problems that you, yourself, have noticed.
Dr. Cohen: So it wasn't surprising. It sort of matched up. I think it would have been more surprising if you're noticing something and I can't find it on my test- then we'd say, ‘what's going on?’ So we're in agreement here
Dr. Cohen: But we said, ‘okay, there's lots of things that can cause memory problems’. We worry about Alzheimer's disease as we get older, but let's rule out other things because there are lots of other causes.
Dr. Cohen: So you did some blood work. So there's no abnormalities in your blood work. Your thyroid is working well, your kidneys are working, your blood counts are normal, your blood sugar is normal. All these things, which are important to check, are good. So I'm glad that the blood work is normal, but it doesn't give us an answer for the memory problem.
Dr. Cohen: So you did another test, An MRI scan. Do you remember having that scan?
Mrs. Olsen: Oh, yes. Yes.
Dr. Cohen: Was that okay?
Mrs. Olsen: Debbie was with me.
Dr. Cohen: She drove you there? Stayed with you? Okay. And you got through the scan okay.
Dr. Cohen: And what the scan shows is a little bit of age related change. So no strokes, no tumors, no scars in the brain, a little bit of shrinkage of the brain, which we expect as we get older. So it doesn't really add up to a diagnosis. A little bit of what we would put down to hardening of the arteries or the small blood vessels in the brain. Again, not enough to explain the memory problem. So what we're left with is a lot of tests that are normal. That's good.
But the memory problem, that's enough to affect some of your day to day activities. And so, we say you have mild dementia, but we still need to rule out other things and that big one to rule out is Alzheimer's.
And we haven't done that yet.
Dr. Cohen: Have you heard of Alzheimer’s disease?
Mrs. Olsen: Yes- but are you sure it's dementia? I mean, what's going to happen to me?
Dr. Cohen: Yeah. That's- it's a tough one. So what I'm telling you now is basically what you know already, there's some things that are more challenging to do because of the memory problem. I can see those on the cognitive tests, but the bloodwork and the MRI scan are not giving us the reason for it.
Dr. Cohen: If this is Alzheimer's- we haven't proven that yet, but if it is- that's a challenging disease because it's slowly progressive and we don't have a cure. But it's still better to know what we're dealing with because there are some treatments and there will be more to come. And we can talk in a lot of detail about how to keep you the best you and keep you happy and doing things you enjoy at home for as long as possible.
Debbie: So what kind of tests will we do?
Dr. Cohen: Yeah. So Debbie, the next tests that I'm going to suggest for mom- and if you're willing- is that we do a spinal tap. So this is a test that we'll do right here in the clinic. There'll be another doctor who's going to do it.
Dr. Cohen: And we're going to just put a little bit of freezing in the back with a skinny needle, take some fluid from around the spinal cord. We don't go into the spinal cord. We'll walk you through it. You'll be great. It sounds worse than it is. And that spinal fluid will give us very important information about whether Alzheimer's disease is taking hold and is the explanation for the memory problem.
Music plays
Mrs. Olsen completed her testing and she and her daughter return to see Dr. Cohen to discuss the results of her full diagnostic evaluation.
Dr. Cohen: Hi, Mrs. Olsen. Good to see you back again. Hi Debbie, thanks for coming in. Great to have you here.
How are you doing?
Mrs. Olsen: I'm doing better- I think.
Dr. Cohen: Oh, good. So the reason we're back today is to talk about the spinal fluid results.
Dr. Cohen: Do you remember having the spinal tap?
Mrs. Olsen: Oh, yes- yes, I do. It wasn't as bad as I thought it would be.
Dr. Cohen: Good. Good.
Debbie: Yeah, You nailed it.
Dr. Cohen: Yeah. I think most people are a little anxious, but when they're doing it, it's actually not too bad.
Mrs. Olsen: I was more worried, I think, about it the night before.
Dr. Cohen: Understood. But you got through it
Dr. Cohen: And the spinal fluid was sent to the lab and has given us some very important and helpful information. So that's what I want to talk to you both about today. So you will remember that we were wanting to get the spinal fluid to help us figure out whether Alzheimer's disease might be the cause of your memory problem.
Dr. Cohen: Okay. So this common and serious disease called Alzheimer's disease; we can actually see in the spinal fluid whether it's there or not, whether it's in the brain. So in your spinal fluid, we do see the changes that are consistent with Alzheimer's. So, yeah, that's maybe not what you were hoping to hear.
Mrs. Olsen: Are you sure?
Dr. Cohen: We are sure.
Dr. Cohen: There are three markers we look at and the earliest changes are there and the other markers are also there. So amyloid is a protein that accumulates really early in Alzheimer's disease. It accumulates in the brain. And we see a level in your spinal fluid that is very consistent with Alzheimer's disease. And there are other markers as well that that give us a sense of certainty that we do have the diagnosis right.
Debbie: How fast will it continue?
Dr. Cohen: So the spinal fluid results don't necessarily tell us how fast things are going to progress. And even though you've had the memory problems for a while, you're at home, you're enjoying your garden and family and doing lots of things. And Debbie's been very helpful for the things that have been a little bit challenging.
Dr. Cohen: And my hope is that the progression of this disease, Alzheimer's disease, will be slow in you. It often is a very slowly progressive disease and that you'll have still lots of time to enjoy things.
But there are there are different things that we can do, you know, treatment wise, and in terms of support services and managing to make sure that you're safe, you're comfortable, and that you have what you need.
Dr. Cohen: And regular follow up with me as well to monitor how this disease is going. So I'm not expecting anything to change tomorrow or next week, next month. But we have a diagnosis here that we know is one of a progressive disease. So we do need to make sure you have the support you deserve and the treatment options that will be available to you.
Music plays
Communicating a Diagnosis of Alzheimer’s Disease with Mild Dementia in Clinical Practice
Dr. Sharon Cohen demonstrates effective communication during the clinical assessment and a diagnosis of a patient living with Mild Dementia from Alzheimer’s disease.
Music plays
Dr. Cohen: There are a number of things that can help make it easier to give a diagnosis. And one thing up front is to be clear that Alzheimer's disease is in a differential diagnosis; that we're not sure that's what we're dealing with. But let's go in a stepwise fashion and cast the net broadly. But keep in mind that Alzheimer's disease is one thing that we will be thinking about ruling out.
Dr. Cohen: I deliver that information very early on when I’m first taking a history. I'm asking people what's going on with their memory and what are they worried about? And some people will tell you upfront, mom had Alzheimer's, or I'm worried I might be developing Alzheimer's, or is this dementia? So, they are asking you already, and that is a great segway to say that is a possibility.
Dr. Cohen: Let's go further. Let's dig deeper. So, you've already planted the seed. That's one of the things that you're considering. As you go through, then with a stepwise cognitive exam and ruling out things with the routine blood work and structural image of the brain. Then, if those tests to look for a cause of a memory problem are not showing any non-Alzheimer's cause, then it's time again to have the conversation about what we've ruled out.
But we haven't yet ruled out Alzheimer's disease. And let's move on and talk about the ways that we can be more specific and more certain.
Music plays
Best Practices for Communicating a Diagnosis in Clinical Practice – AD as a Differential Diagnosis
When evaluating a patient with cognitive impairment, it is important to consider Alzheimer’s disease in the differential diagnosis.
Music plays
Dr. Cohen: In order to have these conversations successfully, the clinician needs to make time. And even though we're all busy, we're all overloaded, when the patient and family are in front of you, you have to compose yourself such that they are the priority. The phone is not ringing. Nobody's knocking on your door to hand you files or charts. The patient and the family member are those important people who you're speaking with, and this conversation cannot be limited to a few minutes.
Dr. Cohen: You can't just say, this is what I think it is, and here are the tests we're going to do, because then you will lose the opportunity not only to reflect on, validate what your patient's feeling, but also to understand better how this disease or the concern about Alzheimer's is impacting their day-to-day life. So, there's valuable information to be gleaned in extended conversations.
Dr. Cohen: None of us have tons of time, but you have to carve out enough time in your day for this conversation. And then you need to have successive conversations where you build on the information, you recap what you've talked about, reinforce what we've achieved so far, and where we're still heading in terms of clarification.
Music plays
Communicating a Diagnosis of Alzheimer's Disease in Clinical Practice - Keeping Your Patient the Priority
Using compassionate communication and allotting adequate time for the diagnosis is a valuable part of making the patient the priority.
Music plays
Dr. Cohen: “Make sure that you have the important people present; and that can be challenging. Even for somebody with mild cognitive impairment who gives their own history very coherently, it is helpful to have them bring a family member or somebody of their choosing to sit in on a diagnostic disclosure, because this is a condition and a diagnosis that will affect not just the patient but the family; and there will be different perspectives. And again, even at the stage of mild cognitive impairment or mild dementia, the individual with a memory problem may not be remembering everything that is necessary to incorporate in the discussion and the treatment plan, and they may not remember everything that's been said at the visit. I can assure you they will take away the sense of empathy, the comfort of the visit or discomfort, if it's an uncomfortable visit.”
“So, the mood is important, and being supportive, empathic is very important; but the details are also important. So having a family member there goes a long way. And I often ask people, are there others who we should invite into the conversation, either now patch them in by phone, or bring them in later, to make sure that we're building the support network for the for the patient.”
Music plays
Communicating a Diagnosis of Alzheimer's Disease in Clinical Practice - Including Care Partners
Ensuring care partners are present in the disclosure of a diagnosis is a crucial step for preparing the patient for the future and building a support network.
Music plays
Dr. Cohen: Patients are people. They come from all walks of life. They have all degrees of education or lack thereof. They have all kinds of anxieties or, you know, different personalities.
Dr. Cohen: And we as physicians are used to being flexible. But in this disease, there are particular sensitivities. People feel threatened when their cognition’s at risk. They worry about what the future will look like, about being dependent on their family, losing things that are dear to them, whether it's driving or being able to recognize their grandchildren. These are precious, precious things that people worry about and worry about much in advance of those stages of disease happening.
So it's important to address these, and it's important to recognize that it's not one conversation that is rolled out in cookie cutter fashion by a physician with each patient and family. It is very much geared to what that patient wants to hear. I don't mean that whether they want to hear good news or bad news, everybody wants to hear good news, how much they want to know, the extent of the detail.
Some people really want to know, what is my amyloid level or can you show me my MRI scan? I want to see that and be willing to share as much information as people want and be respectful that not everybody wants to hear a lot of detail and that it might be upsetting for them. And you have to dole out information in smaller fractions. I deal with the family who says, oh, no, mom would be crushed if she heard she had Alzheimer's disease. You can't tell her. By saying that I have to be honest with my patients I'll be gentle. I don't force a diagnosis down anybody's throat, but I do tell them honestly what I feel they have, and then we move forward. And I don't need to keep reminding them of the diagnosis if that's not helpful. But at least we've said on one occasion what this is.
Music plays
Communicating a Diagnosis of Alzheimer's Disease in Clinical Practice - Acknowledging Patient's Needs
During the diagnosis, it is important to adapt the communication method based on the patient’s need.
Introspective music plays
Dr. Cohen: People feel threatened when their cognition’s at risk. They worry about what the future will look like, about being dependent on their family, losing things that are dear to them, whether it's driving or being able to recognize their grandchildren.
These are precious, precious things that people worry about, and worry about much in advance of those stages of disease happening.
So, it's important to address these, and it's important to recognize that it's not one conversation that is rolled out in cookie cutter fashion by a physician with each patient and family.
Voiceover:
Communicating a diagnosis of Alzheimer’s disease can be challenging. In this video series, we introduce key considerations to address these barriers for communicating a diagnosis to a patient with AD.
Silence
Voiceover:
These five steps for communication are techniques to optimize communication with a patient, based on peer reviewed research and expert best practices.
Voiceover:
The series of educational videos provide advice on techniques using this communication approach together with best practices and excerpts of clinical diagnosis disclosures by Dr. Cohen.
Introspective music plays
Dr. Cohen: Make sure that you have the important people present. And that can be challenging.
Even for somebody with Mild Cognitive Impairment who gives their own history very coherently,….
Dr. Cohen: ….it is helpful to have them bring a family member or somebody of their choosing to sit, sit in on a diagnostic disclosure because this is a condition and a diagnosis that will affect not just the patient but the family, and there will be different perspectives.
Voiceover:
The second patient is Mr. Harris accompanied by his wife. He will later be diagnosed with Mild Cognitive Impairment due to AD.
Jen: Well, you're- you're a little worse off than your friends. Remember when you didn't want to go to the card game?
Mr. Harris: Yeah.
Jen: Because you couldn't keep track.
Mr. Harris: Yeah.
Dr. Cohen: Yeah. And even mild memory problems can make us feel not quite at our best and holding back. So that's understandable.
Dr. Cohen: And many of us joke about, you know, senior moments, as you said, or, you know, we all forget things. But some of us are on the path to a very common disease like your mom, to Alzheimer's.
And so we shouldn't ignore that.
Dr. Cohen: And there are other things that can cause memory problems as well. So, yes, anyone who’s worried about their memory should get it checked out.
Dr. Cohen: The mood is important and being supportive, empathic is very important, but the details are also important. So having a family member there goes a long way.
Dr. Cohen: And I often ask people, are there others who we should invite into the conversation, either now patch them in by phone, or bring them in later to make sure that we're building a support network for the patient.
Dr. Cohen: What about your- you have adult children. You might want to bring them into the conversation. Have you-?
Jen: Yeah, we could tell them. I mean, they could see that there was something going on, but, yeah, I would like them to be a part of this, to know. I don't want to scare them.
Dr. Cohen: Right, right.
Jen: You know, but.. Yeah.
Dr. Cohen: They will probably be reassured to know that dad's getting you know, thorough investigation, that the problem's been taken seriously, but also to hear that the problem's still at a mild stage and that there are things we can do. And to the extent that you're comfortable bringing them into the conversation, they they will probably appreciate that.
Mr. Harris: Yeah.
Jen: Right.
Dr. Cohen: And everybody will benefit and you in particular from having them on side and supportive.
Mr. Harris: Yeah.
Introspective music plays
Voiceover:
Mr. Harris' memory has begun to exhibit signs of decline. Complicating matters is the knowledge that Mr. Harris' mother battled Alzheimer's disease.
Mr. Harris: My mom had dementia. You know, our friends, you know, we kind of laugh about it, you know, We call it our, you know, our senior moment, so.
Dr. Cohen: And again, even at the stage of Mild Cognitive Impairment or mild dementia, the individual with a memory problem may not be remembering everything that is necessary to incorporate in the discussion and the treatment plan. And they may not remember everything that's been said at the visit.
Voiceover:
In this series, you're meeting two patients being evaluated for Alzheimer’s disease. The first patient is Mrs. Olsen who will later be diagnosed with Mild AD.
Voiceover:
Mrs. Olsen came to see Dr. Cohen because she started noticing problems with her memory and has increasingly relied on the caring assistance of her daughter, Debbie.
Dr. Cohen: Hi, Mrs. Olsen. Great to see you again.
Hi, Debbie. Thanks for coming. Appreciate it.
How have you been since I last saw you?
Mrs. Olsen: Oh, I think I'm doing pretty good.
Dr. Cohen: Oh, good, good. I'm glad. Yes. You're checking with Debbie? Yes? She's doing okay?
Dr. Cohen: So we're here to talk about some test results. You had come to me a few weeks ago telling me about your memory not being so strong and worried that something was going on and you were having trouble paying your bills.
Dr. Cohen: So Debbie's been helping with that. And you were having trouble remembering your medicines. So again Debbie stepped up. She's helping. This is good, this is sensible.
Planning Ahead: Engaging Loved Ones
Dr. Sharon Cohen emphasizes the importance of including care partners in the clinical diagnosis discussion and addresses key barriers in communication.
Introspective music plays
Voiceover:
These five steps for communication are techniques to optimize communication with a patient. Based on peer reviewed research and expert best practices,….
Voiceover:
this approach aims to support honest and empathic conversation while sharing the diagnosis.
Voiceover:
The series of educational videos provides advice on techniques using this communication approach together with best practices and excerpts of clinical diagnosis disclosures by Dr. Cohen.
Introspective music plays
Dr. Cohen: In order to have these conversations successfully,….
Dr. Cohen: ….the clinician needs to make time. And even though we're all busy, we're all overloaded, when the patient and family are in front of you, you have to compose yourself such that they are the priority.
Dr. Cohen: The phone is not ringing. Nobody's knocking on your door to hand you files or charts. The patient and the family member are those important people who you're speaking with….
Dr. Cohen: ….and that this conversation cannot be limited to a few minutes. You can’t just say “This is what I think it is, and here are the tests we’re going to do”, because then you will lose the opportunity….
Dr. Cohen: ….not only to reflect on, validate what your patient's feeling, but also to understand better how this disease or the concern about Alzheimer's is impacting their day to day life.
Voiceover:
In this series, you're meeting two patients being evaluated for Alzheimer’s disease. The first patient is Mrs. Olsen, who will later be diagnosed with mild AD.
Voiceover:
In their first visit together, Dr. Cohen completed some brief cognitive assessments with Mrs. Olsen and requested some additional tests.
Voiceover:
Mrs. Olsen completed all the tests and is returning to see Dr. Cohen with her daughter, Debbie.
Dr. Cohen: Hi, Mrs. Olsen. Good to see you back again. Hi, Debbie.
Debbie: Hi
Dr. Cohen: Thanks for coming in. Great to have you here.
Dr. Cohen: How are you doing?
Mrs. Olsen: I’m doing better, I think.
Dr. Cohen: Oh, good.
Dr. Cohen: I’m glad to hear that but in what way?
Mrs. Olsen: Ohh. I don’t know. I guess maybe I feel a little bit more reliable that I can remember things.
Dr. Cohen: Oh good
Mrs. Olsen: Or I think I remember things.
Dr. Cohen: Well, if you're feeling good, let's go with that. That's great. That's great.
Dr. Cohen: So, the reason we're back today is to talk about the spinal fluid results. Do you remember having the spinal tap?
Mrs. Olsen: Oh, yes, yes, I do.
Dr. Cohen: Yes?
Mrs. Olsen: It wasn't as bad as I thought it would be.
Dr. Cohen: Good. Good.
Debbie: And you nailed that.
Dr. Cohen: Yeah. I think most people are a little anxious and then they do it, it’s- it's actually not too bad. So-
Mrs. Olsen: I was- I was more worried, I think, about it the night before.
Dr. Cohen: Understood, understood.
Mrs. Olsen: But it was okay.
Dr. Cohen: Well, that's good. You got through it. And the spinal fluid was sent to the lab and has given us some very important and helpful information. So that's what I want to talk to you both about today.
Dr. Cohen: So, there's valuable information to be gleaned in extended conversations. None of us have tons of time, but you have to carve out enough time in your day for this conversation.
Dr. Cohen: And then you need to have successive conversations where you build on the information, you recap what you've talked about, reinforce what we've achieved so far and where we're still heading in terms of clarification.
Voiceover:
The second patient is Mr. Harris. He will later be diagnosed with Mild Cognitive Impairment due to AD.
Voiceover:
Mr. Harris’ memory has begun to exhibit signs of decline. Mr. and Mrs. Harris have met with Dr. Cohen about these concerns. She has administered a cognitive test and requested some bloodwork and an MRI scan to exclude causes other than Alzheimer's.
Voiceover:
Today, Mr. Harris, and his wife, Jen, are meeting with Dr. Cohen to talk about the test results and seek further insight and guidance.
Dr. Cohen: It’s really good to see you.
So, the last time I saw you, we were sending you off for an MRI scan.
Dr. Cohen: How did that go?
Mr. Harris: Well, it was actually kind of noisy, you know, a little bit scary. You know, and you have to be like, really still, you know?
So, I had to go to the beach. I had to go somewhere where- Hawaii or something.
Dr. Cohen: Yeah. I usually just think of the beach. So, yeah, I can relate. Glad you got through it. That's good.
Dr. Cohen: Okay, so I want to tell you about the MRI results, the blood tests, and also talk about the cognitive testing. So how did we get to this point?
Dr. Cohen: You had come to me not too long ago saying that over the last couple of years, something was changing with your memory.
Dr. Cohen: You're still functioning well, still working in investments. Yes? Okay and still engaged in family life and driving, doing everything independently. But something was changing in your memory. Maybe a little bit of trouble coming up with people's names as well. And just not sure if this was important to tackle or not. But your mom had dementia so that sensitized you to the fact that maybe we should look into this.
Introspective music plays
Open Conversation with a Listening Ear
Dr. Sharon Cohen demonstrates effective communication during the clinical assessment and diagnosis of a patient with Alzheimer’s disease with Mild Dementia.
Introspective music plays
Voiceover:
These five steps for communication are techniques to optimize communication with a patient. Based on peer is ireviewed research and expert best practices,….
Voiceover:
….this approach aims to support honest and empathic conversation while sharing the diagnosis.
Voiceover:
The series of educational videos provide advice on techniques using this communication approach together with best practices and excerpts of clinical diagnosis disclosures by Dr. Cohen.
Introspective music plays
Dr. Cohen: There are a number of things that can help make it easier to give a diagnosis. And one thing up front is to be clear that Alzheimer's disease is in the differential diagnosis, that we're not sure that's what we're dealing with, but keep in mind that Alzheimer's disease is one thing that we will be thinking about ruling out.
Dr. Cohen: …
I deliver that information very early on when I’m first taking a history.
I'm asking people what's going on with their memory and what are they worried about? And some people will tell you upfront, “mom had Alzheimer’s” or “I'm worried I might be developing Alzheimer’s” or “is this dementia?”
Dr. Cohen: So they are asking you already and that is a great segway to say “that is a possibility.
Let's go further. Let's dig deeper.” So you've already planted the seed. That's one of the things that you're considering.
Voiceover:
In this series you're meeting two patients being evaluated for Alzheimer’s disease. The first patient is Mrs. Olsen.
Voiceover:
In their first visit together, Dr. Cohen completed some brief cognitive assessments with Mrs. Olsen and requested some additional tests.
Voiceover:
Mrs. Olsen completed all the tests and is returning to see Dr. Cohen with her daughter, Debbie.
Voiceover:
However, the tests until now have not given the answers to the memory problem.
Dr. Cohen: Have you heard of Alzheimer's disease?
Mrs Olsen: Yes, but are you sure it's dementia? I mean, what's going to happen to me?
Dr. Cohen: Yeah. So… you… yeah, that's that's that's a tough one.
Dr. Cohen: So, what I'm telling you now is basically what you know, already there's some things that are more challenging to do because of the memory problem. I can see those on the cognitive tests, but the blood work and the MRI scan are not giving us the reason for it. If this is Alzheimer's, we haven't proven that yet.
Dr. Cohen: But if it is, that's a challenging disease because it's slowly progressive and we don't have a cure. But it's still better to know what we're dealing with because there are some treatments and there will be more to come. And we can talk in a lot of detail about how to keep you the best you and keep you happy and doing things you enjoy at home for as long as possible.
Voiceover:
Building an empathic conversation about the diagnosis offers several well-known benefits.
Voiceover:
The second patient is Mr. Harris.
Voiceover:
After the previous testing for his memory concerns, he completed a PET scan ordered by Dr. Cohen.
Voiceover:
He and his wife now return to see the doctor and discuss the results of his full diagnostic evaluation.
Dr. Cohen: George, Jen, great to see you again.
Mr. Harris: Good to see you.
Dr. Cohen: Very glad to see you. Yes. So just to recap, we're here to talk about the PET scan results. And we talked about the fact that you have mild cognitive impairment. The MRI and the blood work weren't showing us the cause. We wanted to dig deeper and see, is this Alzheimer's disease. So that's what we're here to talk about.
Introspective music plays
Dr. Cohen: So, the PET scan does show this protein amyloid accumulating. And I know that's not what we were hoping for, but it is the reality that amyloid plaque is developing in the brain. And amyloid is that early, early change of Alzheimer's disease.
Dr. Cohen: So how are you doing with that?
Mr.Harris: [Sighs]. Now, you know… [Sighs] I was really hoping that it would be a different result.
But I… I had a feeling.
Dr. Cohen: You kind of felt that if… it might show Alzheimer's and yet, of course, we're hoping for something else.
Mr. Harris: Yeah. Yeah. This is it's it’s going to be it's going to be difficult.
Dr. Cohen: You know, this is a tough disease. Alzheimer's. But again, you've caught it early.Which is good because there's lots you're doing. You're independent, as we've said before, you're living your life. There's lots to enjoy and do
Dr Cohen: nd our job is now knowing that this Alzheimer's process is brewing.
Mr. Harris: Yeah
Dr. Cohen: To keep you functioning as well as possible as long as possible. So that's my goal for you, and I'm sure that's what you and, and what Jen wants for you.
Introspective music plays
Jen: So we would be okay with leaving him alone. I know that's like kind of far off, but.
Dr.Cohen: Right
Jen: Is he okay being in the house by himself?
Dr.Cohen: He is fine. He is fine at home.
Jen: Okay
Dr.Cohen: And arhh arhh, good that you ask, though, because when we talk about Alzheimer's disease, people often think right away of someone very disabled. Right. And they don't realize this is a very slowly progressive disease that starts almost imperceptibly.
Introspective music plays
Building and Communicating Empathy
Dr. Sharon Cohen elaborates on the importance of cultivating and expressing empathy while maintaining clarity.
Introspective music plays
Voiceover:
These five steps for communication are techniques to optimize communication with a patient.
Voiceover:
Based on peer reviewed research and expert best practices, this approach aims to support honest and empathic conversation while sharing the diagnosis.
Voiceover:
The series of educational videos provides advice on techniques using this communication approach, together with best practices and excerpts of clinical diagnosis disclosures by Dr. Cohen.
Introspective music plays
Dr. Cohen: Patients are people. They come from all walks of life. They have all degrees of education or lack thereof.
Dr. Cohen: They have all kinds of anxieties or, you know, different personalities. And we as physicians are used to being flexible. But in this disease, there are particular sensitivities. It's important to recognize that it's not one conversation that is rolled out in cookie cutter fashion by a physician with each patient and family.
Dr. Cohen: It is very much geared to what that patient wants to hear, how much they want to know, the extent of the detail. Some people really want to know, ‘what is my amyloid level’ or, ’can you show me my MRI scan? I want to see that.’ And be willing to share as much information as people want, and be respectful that not everybody wants to hear a lot of detail and that it might be upsetting for them and you have to dole out information in smaller fractions.
Voiceover:
In this video, you will accompany Mrs. Olsen during the follow up visit for her memory problems. Most recently, she completed a spinal tap ordered by Dr. Cohen.
Voiceover:
Mrs. Olsen completed her testing and she and her daughter returned to see Dr. Cohen to discuss the results of her full diagnostic evaluation.
Dr. Cohen: The spinal fluid was sent to the lab and has given us some very important and helpful information. So that's what I want to talk to you both about today.
Dr. Cohen: So you will remember that we were wanting to get the spinal fluid to help us figure out whether Alzheimer's disease might be the cause of your memory problem. Okay.
Dr. Cohen: So this common and serious disease called Alzheimer's disease, we can actually see in the spinal fluid, whether it's there or not, whether it's in the brain.
Dr. Cohen: So in your spinal fluid, we do see the changes that are consistent with Alzheimer's. So, yeah, that's maybe not what you were hoping to hear.
Mrs. Olsen: Are you sure?
Dr. Cohen: We are sure. There are three markers we look at and the earliest change is there and the other markers are also there. So amyloid is a protein that accumulates really early in Alzheimer's disease. It accumulates in the brain, and we see a level in your spinal fluid that is very consistent with Alzheimer's disease. And there are others markers as well that that give us a sense of certainty that we- we do have the diagnosis right.
Introspective music plays
Voiceover:
The second patient is Mr. Harris, accompanied by his wife. Last video, Mr. Harris was diagnosed with Mild Cognitive Impairment due to AD.
Voiceover:
We now return to see the continuation of the discussion with Dr. Cohen.
Mr. Harris: So, how do I stay my best self? I mean, you know, I don't want to forget about my kids. I don't want to forget about my grandkids.
Dr. Cohen: Of course, family is important and our memories are precious.
Mr. Harris: Yeah.
Dr. Cohen: So, you know, you're right to to be you know, asking me this.
Mr. Harris: Yeah.
Dr. Cohen: Fortunately, as I said, you've caught this early; that gives us the best chance to try and keep this stable.
Mr. Harris: Yeah.
Dr. Cohen: What we're dealing with is a slowly progressive disease. So we're not talking about, you know, suddenly falling off the cliff. We're talking about changes happening very gradually, and you may have still several more years of doing everything just about the same as now.
Dr. Cohen: But we will have a session to talk much more about strategies to keep you living well, possible medicines that might be helpful, and, you know, what's the best way to manage, knowing that we have the diagnosis and having this diagnosis is what opens the door then to treatment options and not sending us down the wrong path or minimizing or ignoring.
Introspective music plays
Patient-Centric Communication when Sharing the Diagnosis
Dr. Sharon Cohen explores the concept of patient-centered communication during diagnosis disclosure, recognizing that each patient may have unique preferences for the information they receive.
Dr. Ortega has been practicing medicine for fifteen years and has experience with frustrated patients trying to understand if their declining faculties are normal aging or something more.
Presenting patients and their families with a diagnosis of Alzheimer’s disease can be hard for many reasons, including:
- the substantial time and preparation required
- the impact on patients and their loved ones
- uncertainty about the diagnosis
- and, finally, the limited number of effective treatments.
Given all that, Dr. Ortega understands why some HCPs are reluctant to have these conversations.
But, he also knows the many benefits of direct and honest communication with his patients and their loved ones.
Let’s follow Dr. Ortega as he plans ahead to inform Linda that she’s in the early stages of Alzheimer’s disease.
Dr. Ortega’s schedule is full, but he’s adamant that enough time be set aside so patients can ask questions and get satisfactory answers.
Before the meeting, he reviews the data supporting Linda’s diagnosis and will have it on hand to help explain test results.
Dr. Ortega bolsters himself by remembering the beneficial outcomes these conversations can have.
Patients and their families are often aware the patient is having issues with memory and thinking, and finally having an explanation can help validate their concerns.
Providing clear, truthful, and helpful information will strengthen the HCP-patient connection, which will be crucial as management gets more complex over time.
Having a diagnosis broadens a patient’s access to treatments—both pharmacological and non-pharmacological—and referrals to related specialties.
Early diagnosis also gives patients the chance to understand their disease and learn coping skills before new symptoms arise. This gives them more time to plan ahead, communicate their wishes, and arrange for supportive care measures when needed.
Showing empathy when communicating with patients has many benefits, including a positive impact on patient satisfaction and adherence to treatment.
That’s why Dr. Ortega addresses questions as they arise, uses empathetic statements to recognize Linda’s emotions, and engages with a willingness to help.
Communicating a diagnosis of Alzheimer’s disease will never be easy for any of the participants.
But, with the right preparation and tools, it can strengthen the HCP-patient connection to improve continued care.
With early, empathic, patient-centered communication, HCPs can help patients and their loved ones accept the diagnosis of Alzheimer’s disease, consider effective strategies treatments, and together, actively plan for the future to maintain independence and quality of life for as long as possible.
Improving Communication in Diagnosis of Early Alzheimer’s Disease
A whiteboard animation which describes the key strategies an HCP should utilize to optimize their communication of an Alzheimer's Disease diagnosis.
In the previous video, Dr. Ortega prepared for a conversation with Linda and her daughter about her diagnosis of Alzheimer's disease. He took time to prepare for that discussion because he knows the benefits of direct and honest communication with his patients.
Dr Ortega knows that patients differ in their response to the diagnosis and the amount of information they desire. Therefore, he is prepared to adjust his discussion based on cues from the patient in each individual encounter.
In previous meetings, Linda has wanted all the information about her health and test results.
Dr. Ortega opens his conversation with Linda and her daughter by briefly summarizing what led them to this moment.
“I know you’ve been talking to me about your concerns with your memory and thinking, and we have done several tests together. I am glad that you and your daughter are here together today to talk about the results of those tests.”
Avoiding complex medical terms as much as possible, Dr. Ortega communicates Linda’s diagnosis using realistic, but hopeful, language.
He tells her, “At this point, you are in the early stages of Alzheimer’s disease. It’s good we diagnosed it early because this will give us time to discuss this together, and plan for your future.”
Dr. Ortega pauses frequently when talking to allow Linda or her daughter the opportunity to respond or ask questions.
Careful to make sure Linda doesn’t feeling like she’s being tested, Dr. Ortega leverages the teach-back method in their communication. Having Linda explain details back in her own words helps Dr. Ortega get a better sense of what Linda understands and if he’s communicating in a clear manner.
It is very helpful that Linda brought a loved one with her so that she has someone else listening to Dr. Ortega and asking questions. If she missed something, or misunderstood, her daughter can review the conversation.
At the end of the diagnostic conversation, Dr. Ortega summarizes their conversation and reminds Linda that he’s there to support her.
Depending on Linda’s response to the diagnosis, and interest, he may initiate discussion about next steps, including potential treatments or other management strategies.
At the conclusion of their visit, he reminds Linda and her daughter regarding their plans, and confirms that Linda has his contact information if questions arise.
Dr. Ortega believes that his patients deserve clear and honest communication about the diagnosis of Alzheimer’s disease, even in the earliest stages.
It is a sign of respect to respond to their concerns and pursue a diagnosis, and, once complete, to deliver this news with empathy.
When we enable early conversations, we’re doing what is possible to help patients and their family preserve their independence, plan for their future and optimize their quality of their life for as long as possible.
Best Practices when Communicating a Diagnosis of Alzheimer’s Disease
A whiteboard animation which illustrates the best practices for an HCP when delivering an Alzheimer's Disease diagnosis.
References
- Rasmussen J, Langerman H. Alzheimer's Disease - Why We Need Early Diagnosis. Degener Neurol Neuromuscul Dis. 2019;9:123-130. Published 2019 Dec 24. doi:10.2147/DNND.S228939
- Grossberg GT, Christensen DD, Griffith PA, Kerwin DR, Hunt G, Hall EJ. The art of sharing the diagnosis and management of Alzheimer's disease with patients and caregivers: recommendations of an expert consensus panel. Prim Care Companion J Clin Psychiatry. 2010;12(1):PCC.09cs00833. doi:10.4088/PCC.09cs00833oli
- Yates J, Stanyon M, Samra R, Clare L. Challenges in disclosing and receiving a diagnosis of dementia: a systematic review of practice from the perspectives of people with dementia, carers, and healthcare professionals. International Psychogeriatrics. 2021;33(11):1161-1192. doi:10.1017/S1041610221000119
- This resource was developed by Eli Lilly and Company and Dr. Sharon Cohen, MD, and Prof. Katherine Rankin, PhD, who are experts in Alzheimer's Disease. This work was inspired by established peer reviewed research but created based on the participants’ perspectives and opinions as well as from data on file from multiple Lilly advisory settings.
- Yen PH et al. Fed Pract. 2019;36(6):284-89.
- Wollney EN, Armstrong MJ, Bedenfield N, et al. Barriers and Best Practices in Disclosing a Dementia Diagnosis: A Clinician Interview Study. Health Services Insights. 2022;15. doi:10.1177/11786329221141829
VV-MED-153540
Please rate your satisfaction with the content on the following statements:
Very Dissatisfied
Dissatisfied
Neutral
Satisfied
Very Satisfied