Chronic Lymphocytic Leukemia (CLL)
Considerations for Treatment Selection
Patient Case Materials: HCP infographic/slides
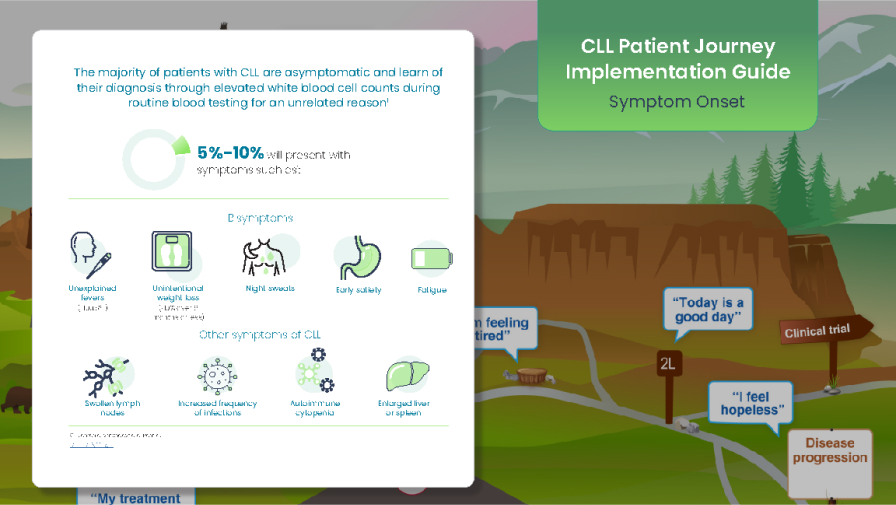
This implementation guide will assist walking the HCP through the CLL patient journey map.
This roadmap is an educational tool about treatment pathways for patients diagnosed with CLL. It is designed to be used in discussions between healthcare professionals (HCPs) and their patients.
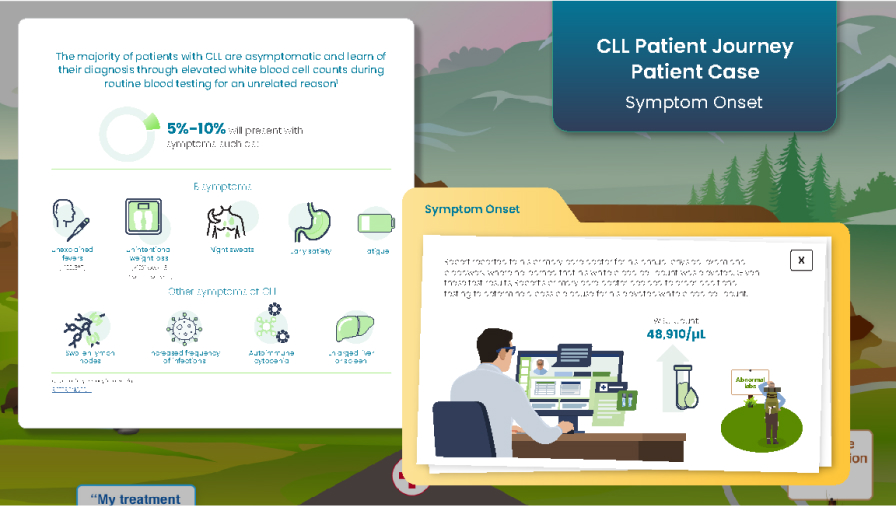
Explore the CLL Journey Map Patient Case, which covers diagnosis, staging, prognostic testing, treatment options, adverse events, and supportive care throughout the treatment journey.
Interactive clinical case: navigate a CLL patient case of a 65-year-old male from diagnosis to treatment selection throughout different lines of therapy.
Videos
CLL Patient Journey Patient Case
CLL patient case study: Dr. Andrew Lipsky discusses the case of a 78-year-old male patient with CLL from diagnosis through third-line therapy.
(0:00-0:23) Headshot and title fade out, and disclaimer and disclosures fade in.
Welcome. My name is Andrew Lipsky. And I’m an assistant professor of medicine at Columbia University Medical Center, where I specialize in caring for adult patients with hematologic malignancies, including chronic lymphocytic leukemia, CLL, and lymphoma.
And my research really focuses on bringing the latest in clinical trials to the care of patients with CLL.
(00:25-00:52) Slide animation
So, in this presentation, I’ll review the case of John, a male patient diagnosed with CLL. In 2024, he was 78 years of age and had previously progressed through 2 lines of therapy. And when discussing 3rd-line options, John was interested in a therapy that really could allow him to maintain his flexible lifestyle.
And so, in today’s discussion, we’ll review John’s CLL treatment history up to this point and how we decided together which 3rd-line therapy was right for him.
(00:53-01:28) Slide Animation
In 2014, John was 68 years of age and had recently retired from his job as a painter. He had a history of hypertension and hyperlipidemia. And during a visit to his primary care provider, routine bloodwork detected a lymphocytosis to 24,000, and physical examination revealed small cervical lymphadenopathy.
After John was referred to a hematologist, the diagnosis of CLL was confirmed with flow cytometry, and an initial prognostic workup revealed unmutated IGHV, with FISH testing notable for the presence of a deletion 11q.
(01:29-01:37)
Because his hemoglobin and platelets were normal and he was otherwise asymptomatic, John was placed on “watch-and-wait” surveillance at that time.
(01:38-02:32) Slide Animation
In 2016, John’s fatigue increased, and his lymphadenopathy worsened. Laboratory evaluation was notable for an increasing lymphocytosis and a new anemia that, after we worked it up, was attributable to CLL.
He began 1st-line therapy with ibrutinib 420 mg once daily, and his lymphadenopathy subsequently resolved with normalization of his hemoglobin.
When John needed to start treatment, the approval of covalent BTK inhibitors for 1st-line therapy in CLL really met an unmet need for targeted therapy in this patient population. And, really, subsequent studies have validated the benefit of targeted therapy over prior chemoimmunotherapy options.
So, when deciding on treatment, I like to educate patients on available options and discuss what factors are important to them.
(02:33-02:39)
I also consider prognostic markers and other patient characteristics that may be important, such as their particular medical comorbidities.
(02:41-04:17) Slide Animation
In early 2021, John’s absolute lymphocyte count began steadily increasing, along with enlargement of multiple axillary and inguinal lymph nodes. Three months later, he developed severe fatigue and recurrent anemia.
So, here, the clinical picture certainly looks like progressive CLL, but it really is important to make sure that the patient's symptoms are indeed attributable to the disease. Work up any anemia, look for other causes of the fatigue, and after this, assess for true progression based on the iwCLL criteria.
Repeated prognostic evaluation with FISH demonstrated the same deletion 11q without the presence of a deletion 17p. Next-generation sequencing showed TP53 wild type but also detected a BTKC481S mutation, with a variant allele frequency of 78%.
Repeating cytogenetic and molecular testing at each line of therapy may help to prognosticate patients and also identify resistance mechanisms to the current line of therapy. But it's important to keep in mind that, really ultimately, it's the symptoms and the patient meeting iwCLL criteria that drives the need for treatment.
And I’d like you to keep in mind, again, that before treating progressive CLL, repeating biomarker testing, such as FISH and karyotype and TP53 status, is just important to prognosticate as patients may experience clonal evolution of the CLL over time.
In John’s case, treatment with venetoclax + rituximab was initiated, with rituximab administered for the first 6 cycles and venetoclax continued for 2 years.
(04:18-05:21) Slide Animation
In 2024, at 78 years of age and after 1 year of being off treatment with CLL, John’s only medications were hydrochlorothiazide and atorvastatin.
At follow-up visits, he demonstrated recurrent lymphocytosis, with subsequent development of lymphadenopathy and splenomegaly, with also the presence of early satiety. His complete blood count also showed concurrent anemia and mild thrombocytopenia.
Repeated risk stratification testing now also revealed the presence of a deletion 17p that had been acquired on FISH testing, as well as next-generation sequencing showing the presence of a TP53 mutation.
So, when thinking about available options for 3rd-line treatment in CLL, it’s certainly exciting that we have new therapeutic modalities for patients already exposed to covalent BTK inhibition and venetoclax. These new options include non-covalent BTK inhibition with pirtobrutinib and cellular therapies with CAR-T cells.
In each case, I think it’s important to take the patient’s disease status, performance status, comorbidities, and life preferences into consideration.
(05:22-05:50) Slide Animation
In this case, John was started on pirtobrutinib at a dose of 200 mg daily. He experienced some mild fatigue, bruising, and diarrhea. But after an initial period of treatment-associated lymphocytosis, his white blood cell count normalized, and he had resolution of his anemia and thrombocytopenia.
At subsequent visits, it was noted that all of John’s laboratory markers had essentially returned to baseline, and he continues to be on treatment as of June 2024.
(05:51-06:01) Slide Animation
So, a few key points can be taken away from this patient case.
Overall, it's clear that we're now in an era of targeted agents that have revolutionized the treatment course for patients living with CLL.
(06:02-07:11)
At each stage of treatment, it's important to fully work up any potential signs of progression, like anemia, and ensure that they're attributable to CLL. It's also important to initiate a discussion of possible treatment options as soon as you see that initial rise in disease activity. You should confirm that you have the most accurate picture of the disease by repeating cytogenetic and molecular testing at progression.
It's critical to educate patients on all available therapeutic options to help them understand what treatment may be available now and what treatment options may be utilized during subsequent progression.
During these discussions of CLL treatment options, patient preferences and characteristics and disease attributes should all be considered to make the appropriate decision for that patient.
And, finally, in the 3rd line, pirtobrutinib represents an FDA-approved option for patients who have previously been treated with a covalent BTK inhibitor and venetoclax.
I want to thank everyone for listening to this patient case presentation. And we hope that the information provided here will positively affect your treatment approach in treating patients with chronic lymphocytic leukemia.
How do you manage resistance and intolerance to targeted therapies in CLL?
Dr. Roeker and Dr. Thompson share their approach on how to manage resistance and intolerance to targeted therapies in CLL.
(00:10) Meghan Thompson:
One thing that comes up for patients already on treatment is that unfortunately some patients do become resistant to the treatment that they're taking and have CLL progression, and need another line of therapy. So there is a lot of testing out there for various different treatment types, to start to look at how do we evaluate resistance, looking at mutations. But I do want to highlight that still, even in this era where some of that testing might be available, what really should be guiding clinicians and what guides me in clinical practice and according to the guidelines, is really is the patient having signs or symptoms of CLL progression, progressive lymph nodes, growth of the spleen, worsening cytopenias, constitutional B symptoms, lymphocytosis, all those disease markers, and the clinician's assessment is really what's key.
(01:12) Lindsey Roeker:
Couldn't agree more. And we have patients who do develop resistance. Unfortunately, we also have patients who are intolerant to the treatments that they're on. So they develop a side effect that becomes problematic enough that we need to stop that medication.
(01:27) Lindsey Roeker:
There are a couple of different strategies, and a lot of it depends on what the actual intolerance is. Are these nuisance side effects that we can deal with by switching to another drug in the same class, or are these really more significant side effects where we need to entirely switch classes? And that is another important consideration. Often when patients are intolerant, we do stop medication for some amount of time to let the adverse event really wash out before we start a new therapy.
(01:59) Lindsey Roeker:
It also highlights that there are patients who are intolerant in the setting of pretty good disease control, and those are patients where you can, on a case by case basis, stop therapy and observe for some amount of time before you need to treat. There are drugs that are intended to be given continuously, but sometimes if patients are developing side effects, that is a reason for discontinuation. You don't always need to rush into the next line of therapy.
(02:25) Lindsey Roeker:
That's significantly different than the case of resistance, where often when you're stopping a therapy in the setting of resistance, the disease pace really will pick up, and that's an important point as well. So if a patient's developing resistance, often keeping them on their drug until you have the next line of therapy in place, is an important piece. Because otherwise you can really develop quick progression without a next line.
(02:54) Meghan Thompson:
Yeah. I think that that's really important. And you hit on something that is just so key for providers to pay attention to, and that it really is, it comes into play in patients who might've had multiple therapies for their CLL, what was the reason for discontinuation of the prior treatment? Was it a side effect, toxicity? Were they intolerant to the medicine and not truly progressing on the medicine but might've had good disease control? Or was it a case where they were taking the medicine or shortly after finishing the therapy if it wasn't continuous, that they actually had true CLL progression with some of the signs and symptoms we talked about? And I usually use that as a guiding principle when selecting therapy.
VV-MED-163244
Please rate your satisfaction with the content on the following statements:
Very Dissatisfied
Dissatisfied
Neutral
Satisfied
Very Satisfied